Congratulations on matching to a fellowship in the most exciting field in ophthalmology!
Once the excitement wears off you might feel nervous - which is completely normal. Retina fellowship is like starting all over again. You’ll be seeing patients that you may have only had to superficially manage before and you’ll be doing surgeries that you’ve never done before.
But don’t worry. At every step of the way - you’ve managed to overcome the obstacles you needed to get to where you are, and retina fellowship will be no exception.
Here is a reading and resource roadmap that might help you get your bearings early on in fellowship.
During Residency
Big Picture: Focus on graduating. Enjoy the company of your co-residents. Enjoy not being stressed about matching.
Start reading https://retinatoday.com/. It’s a great resource to see what’s hot and being talked about in our field. Skim the headlines and read what’s interesting
Finish all the retina questions on the OKAPS question banks. You’ll pass OKAPS, you’ll pass the boards, and you’ll get some of the high yield topics.
Set up the VR surgery modules on the EyeSi (you might not have time in fellowship!) - play around to get a feel for the scope and the pedals. You don’t have to finish all the modules - just get a sense of what’s going on.
Read Vit Buckle Academy https://vba.vitbucklesociety.org/ it takes an hour to go through everything and get the basics.
Shadow some cases in the OR to get a sense of the steps involved in retinal surgery. How are retinal detachments repaired? What are the steps of a macular case? How is a scleral buckle done?
https://eyeguru.org/ has excellent modules for you to practice reading OCTs and fundus photos
During Fellowship
It’s time to start building the knowledge base.
Decide how you want to keep your notes organized. I recommend digital with a notetaking app. I like to use https://obsidian.md/ for my surgical notes/reading notes, apple notes for quick access sticky notes, and https://notability.com/ to store my textbooks that I annotate (it can let you sync PDFs with the cloud). All these things can be accessed on my desktop, laptop, and phone.
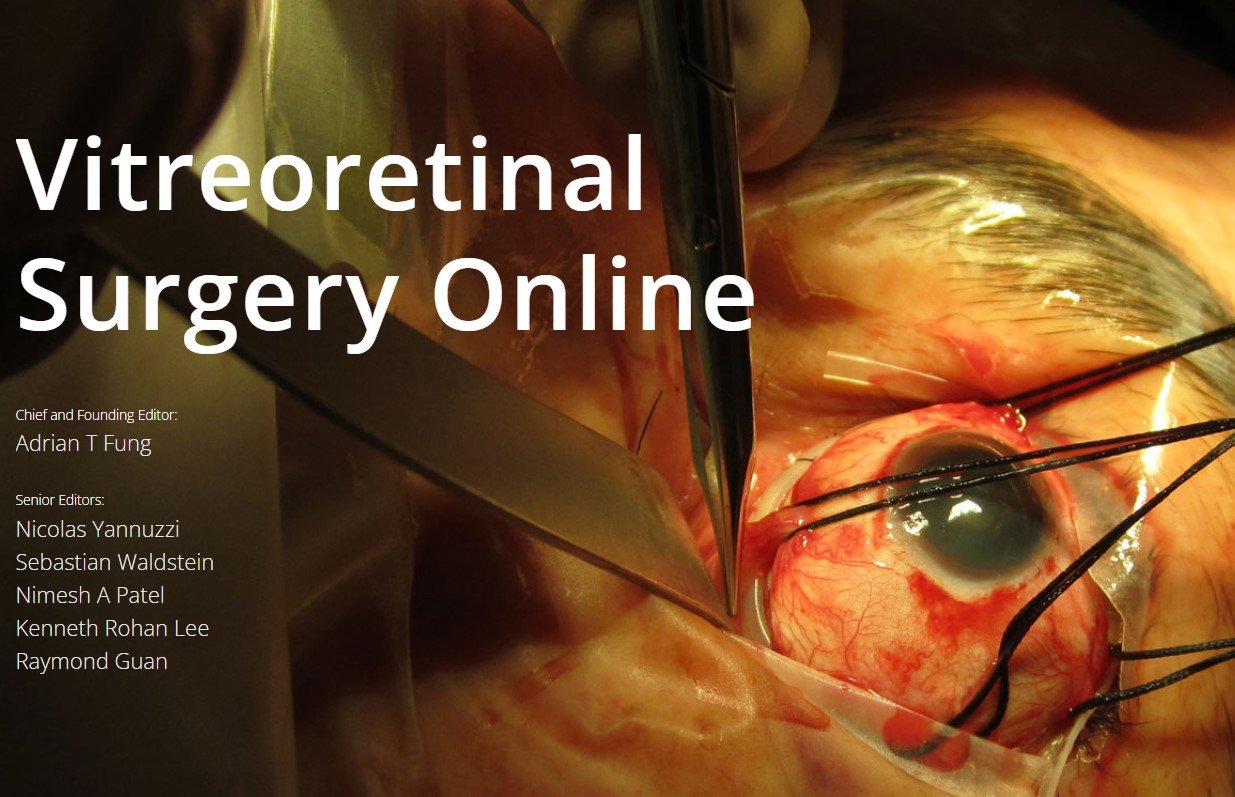
https://www.vrsurgeryonline.com/ is the single greatest retinal surgery resource ever created period. Read the chapters before your cases.
Study BCSC Retina and start being fluent in the wide variety of topics within the field. I would recommend a digital copy if you have one stored on the cloud.
Make a running list of topics that you want to learn about and look them up on - Eyewiki
Find the op-notes of the attendings you are working with and create your own library. This will be useful when you leave fellowship. I use it every day before the OR just to review the steps of surgery
A Deeper Dive (weekend Reads)
Review Articles on https://pubmed.ncbi.nlm.nih.gov/ are a great resource to get a summary of specific topics if Eyewiki isn’t in depth enough
The AAO preferred practice guidelines are an excellent benchmark to base your management on. https://www.aao.org/summary-benchmark-detail/retina-summary-benchmarks-2020
My favorite textbooks are Ryan’s Retina , Duker’s OCT, and the Yannuzzi Retina Atlas. If you are strapped on cash as a poor trainee - there are digital versions that may be able to be obtained until you buy your own copies as an attending.
Listen to podcasts http://www.retinapodcast.com/ and https://eyetube.net/podcasts/new-retina-radio during your commute
Continuing Medical Education
Download BrowZine https://browzine.com/ and follow the major journals. It uses your institution log in to automatically download the updated journal issues.
I created a website https://retinahomepage.com/ that tracks the latest free retina content that can be consumed.
Go to the major retina meetings. Vit Buckle Society, ASRS, and AAO are the ones that you can have access to early in training.
Parting thoughts
Don’t overwhelm yourself. Retina is a lifestyle - not a test that you have to cram for. As long as you maintain your curiosity and strive to be better for your patients - you will learn what you need to know in due time.
Good luck!!
Louie Cai







![Lessons from our Pupils: A Reflection [Podcast Episode 153]](https://images.squarespace-cdn.com/content/v1/58175064c534a576aa3c8f69/1552232851399-1TQEPQO0R12ZLLGXJEIQ/PhysicianonFireWCINetwork.jpg)
